دکتر سیمین دانشور در هشتم اردیبهشت سال 1300 شمسی در شیراز متولد شد. اين بانوی داستان سرا از كودكي با ادبيات و هنر توسط مادر و پدرش آشنا شد. مشوق دانشور در داستاننویسی فاطمه سیاح، استاد راهنمای وی و صادق هدایت بودند.
در سال 1327 با جلال آلاحمد آشنا شد که بعدها با او ازدواج کرد. در سال 1331 به دانشگاه استنفورد رفت و در آنجا دو سال در رشتۀ
زیباییشناسی تحصیل کرد.
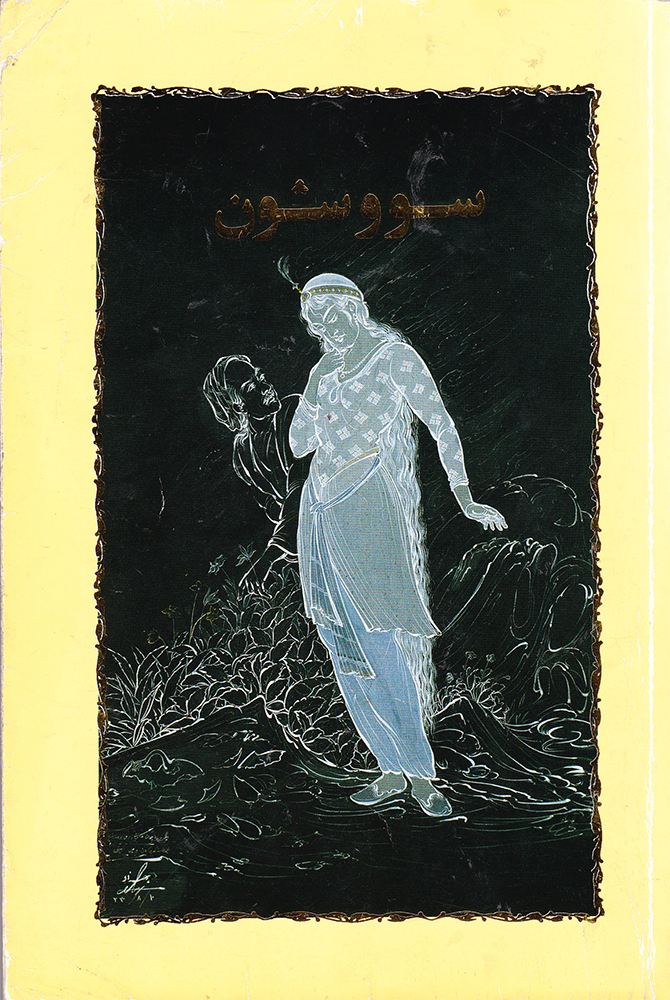
در سال 1348 رمان سووشون را منتشر کرد، که از پرفروشترین رمانهای معاصر است.
دكتر دانشور تا سال 1359 به تدريس در دانشگاه هنر و ادبيات مشغول بود.
اکنون بیست و سه کتاب از او در قالب تألیف و ترجمه چاپ و منتشر شده؛ که مهمترین آنها عبارتند از : آتش خاموش، باغ آلبالو، دشمنان،
کمدی انسانی، داغ ننگ ، شهری چون بهشت، سووشون، بنال وطن، به کی سلام کنم؟، غروب جلال، ماه عسل آفتابی، جزیرهی سرگردانی،
از پرندههای مهاجر بپرس، و ساربان سرگردان.